“A drug that soothes the cravings of dope
sick addicts” was how the Boston Herald
defined methadone in an article this past July.
Would they describe a medication for paralysis
as “a drug to ease hobbling cripples”? Why is
the discipline of addiction medicine subject to
so much derogatory slang terminology? Why
do people continue to use it while words like
crippled, retarded, and crazy have vanished
from medical lexicon?
This stigmatizing vocabulary is not only
stereotyping patients but compromising
the discipline of addiction medicine. A
lawmaker will be less likely to support
“A drug to soothe cravings of dope sick
addicts” than a “medication to treat chemical
dependencies”. Insurance companies, when
choosing what they will cover, would be less
likely to provide coverage for dope fiends or
crack heads. Funding agencies are faced with
similar choices.
During the war on drugs many of these
derogatory terms were introduced into the
vernacular. It was an effort to create a
negative image of the substance, in hope of
dissuading people from using it. Education
took a backseat, mainly because little was
actually known about the subject. As when
little was known about lightning, people
were told the gods were angry. We are now
at a point in science where we understand
what addiction is and no longer need to
scare people toward abstinence by
perpetuating stigmatizing terminology.
Education is proving to be a superior
tool. Using medical terminology in place of
slang, when appropriate, will benefit both
patient and provider. Our effectiveness at
reducing the stigma associated with
addiction will impact the future availability
of funding and treatment. See Breaking the
Stereotype at naabt.org.
Edwin A. Salsitz, MD.,FASAM was one of
the first experts in addiction medicine to
recognize the stigmatizing effects of slang
and urged colleagues to limit the use of it.
See Links at naabt.org to read Dr. Salsitz’s
2002 letter.
SAMHSA has compiled a Guide to the Use
of Language with explanations and
recommendations. This can be downloaded
from our Links page. |

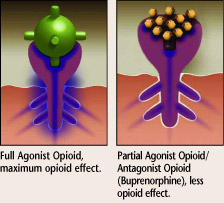
What is it? 
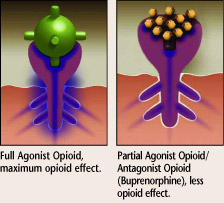
Precipitated withdrawal syndrome (PWS)
can occur when an antagonist (or partial
antagonist, such as buprenorphine) is
administered to someone dependent on full
agonist opioids (hydrocodone, oxycodone,
heroin, methadone, etc.) while still
experiencing agonist effects. Due to
Buprenorphine’s high affinity and low
intrinsic activity at the mu receptor, the partial antagonist displaces agonist opioids
from the receptors, without activating the
receptors to an equivalent degree, resulting
in a net decrease in agonist effect, thus
precipitating a withdrawal syndrome.
What to do about it?
The best way to avoid this condition in
practice is through patient education. Once
the risk of under-reporting last use is
understood, PWS can be avoided. The patient
should be educated, prior to the induction
appointment, of what precipitated
withdrawal is and how they can avoid it.
PWS puts the patient at risk for
concluding that Buprenorphine is
ineffective, the doctor may not know
how to help, or both. Either situation
leaves the patient in a precarious state
physically and emotionally.
If a patient does experience PWS the
common treatment is to increase the dose
of buprenorphine by 2 to 4mgs. hourly,
until symptoms subside. See TIP40 for more
on PWS and the unique pharmacology of
Buprenorphine.
NAABT is completing a sheet for distribution
that will serve as a guide to preventing
precipitated withdrawal. It will be available
for download on our Literature page, or you
may request printed copies be sent to you.
|
 |
11/22/2005 |
|
Depot Buprenorphine
A number of companies are conducting
studies on new forms of buprenorphine
medications to treat opioid addiction.
One – Probuphine – can potentially
provide up to six months of continuous
delivery of buprenorphine. It is placed
subcutaneously in the upper arm area in
15-minute procedure, and removed at the
end of treatment. Another potential product
– Norvex – is comprised of biodegradable
micro pellets administered intramuscularly.
slowly dissolves over a period of 4-6 weeks,
providing a continuously diminishing dose.
Continuous long-term delivery of
buprenorphine may potentially eliminate
some challenges associated with daily oral
therapy, including poor compliance, and
variable blood levels. Both of these drugs are
still in clinical trials and not FDA approved.
See NAABT News page for details.
SAMHSA Releases New Treatment
Improvement Protocol on Medication-
Assisted Treatment for Opioid
Addiction in OTPs
A new Treatment Improvement Protocol,
TIP 43, released in late October by SAMHSA
provides treatment providers, physicians and
other medical personnel with current
information on
medication-assisted
treatment for people
addicted to opioids.
Although this 332-
page volume primarily
focuses on methadone,
many of the same
principles apply to
Buprenorphine.
The PDF version of
the publication is available on the
Literature page at naabt.org. |
|
 |
| National Patient Waiting List and
Physician Matching System
NAABT has developed, and and is currently
testing, a national patient list. This list was
borne out of the need for a more efficient
way to connect patients to certified
physicians. At the same time, it alleviates
the burden of physicians’ maintaining their
own patient waiting lists by allowing them
immediate access to
the NAABT list when
there is an available
treatment opening.
It is completely
confidential. Patients can
get onto the list online
themselves, through the
help of a counselor,
social worker, or other
advocate or organization. It can also serve as
a referral system for physicians.
A physician would log in and see a
list of patients in his/her area currently
awaiting treatment. The patient is asked 15
questions, on a short application. Physicians
can view these answers to determine if a
patient is an appropriate match. If so, an
email is sent to the selected patient(s) with
instructions to call the physician’s office to
discuss treatment further.
A single physician can contact up to 10
patients in less then 3 minutes, by using the
system. Patients can register in under 3
minutes, and are required to respond to a
renewal email every two weeks if they have
not found treatment, maintaining a fresh list.
More will be available on the waiting list
in the coming months.
Read details of the patient waiting list. |
 |
• Advocacy
• Pregnancy and Buprenorphine
• Results of Patient Waiting List Pilot |
 |
| All NAABT literature is available on the
naabt.org Literature page as PDF files
of literature for you to download and
view or print for your convenience. For multiple copies of NAABT
Literature, please email your request
to MakeContact@naabt.org.
The Physician Locator (Doctor/Patient
button) sorts physicians by distance in
geographic proximity, regardless of
city, town, county, or state borders.
Click here to try it for yourself.
Current Newsletters are available at the
naabt.org homepage. Past editions are
available as PDF files on our Literature
page, under Other Literature. |
 |
 |
 |
| The National Alliance of Advocates for
Buprenorphine Treatment is a non-profit
organization formed to help people, in need of
treatment, find treatment providers who are
willing and able to treat opioid dependency in
the privacy of a doctor’s office. Our website offers
answers to frequently asked questions, a glossary,
actual patient experiences, a discussion board,
information on the history and treatments of opioid
addiction, current news on the subject and more. |
|